Total Shoulder Replacement
Summary
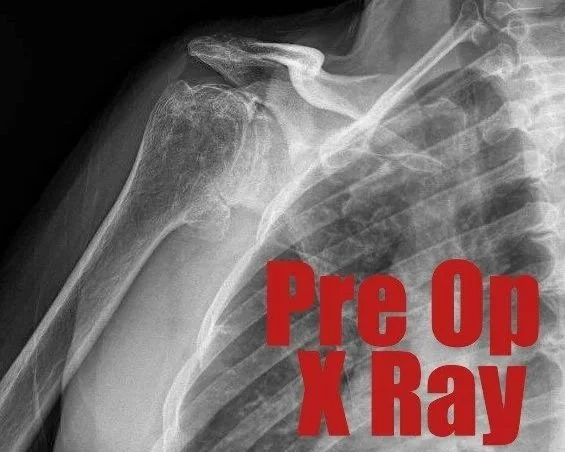
Shoulder arthroplasty, commonly known as shoulder replacement surgery, is a procedure that removes damaged parts of the shoulder joint and replaces them with artificial components (prostheses). The primary goal of this surgery is to alleviate pain and restore function in individuals suffering from severe shoulder joint conditions..
Indications
Shoulder arthroplasty is typically recommended for individuals experiencing persistent and severe shoulder pain, limited motion, or significant interference with daily activities that have not responded to conservative treatments like physical therapy, medication, or injections. Common conditions that lead to shoulder arthroplasty include:
Osteoarthritis: "Wear-and-tear" arthritis, which damages the cartilage covering the ends of bones.
Inflammatory arthritis (e.g., Rheumatoid Arthritis): Caused by an overactive immune system, leading to cartilage and bone damage.
Proximal humerus fractures: Severe fractures of the upper arm bone that may require replacement.
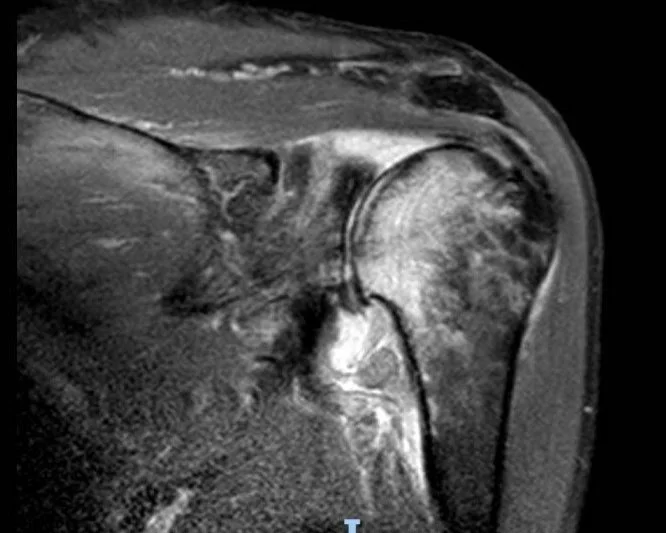
Irreparable rotator cuff tears: Damage to the group of muscles and tendons surrounding the shoulder joint that cannot be repaired.
Rotator cuff arthropathy: Arthritis combined with irreparable rotator cuff tears.
Avascular necrosis (osteonecrosis) of the humeral head: Death of bone tissue due to a lack of blood supply, causing the bone to collapse.
Post-traumatic arthritis
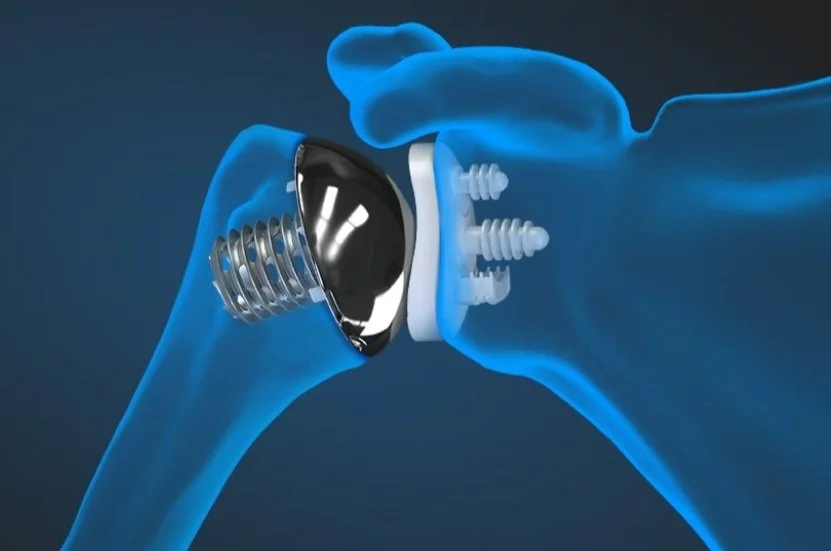
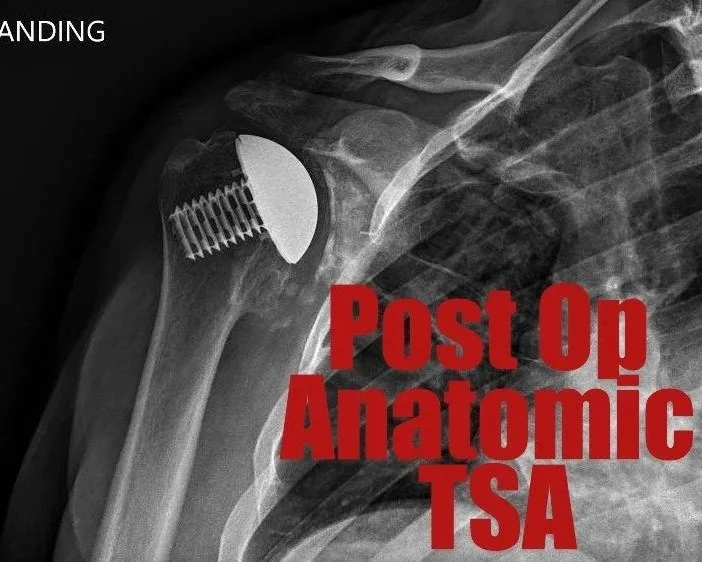
Anatomic Total Shoulder Replacement (TSA): Both the ball of the humerus and the socket of the shoulder blade are replaced with implants that mimic the natural anatomy of the shoulder. This procedure is ideal for patients with severe arthritis and an intact, functioning rotator cuff.
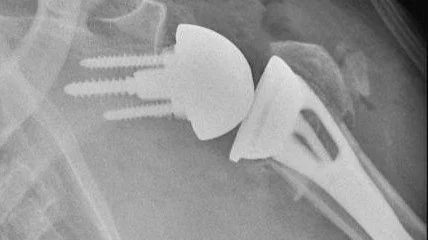
Reverse Total Shoulder Replacement (rTSA): The positions of the ball and socket are reversed. An artificial ball is attached to the shoulder blade, and a socket is attached to the upper arm bone. This type is typically chosen for patients with irreparable rotator cuff tears, severe glenoid wear/deformity, or complex shoulder fractures, as it allows other muscles (like the deltoid) to move the arm when the rotator cuff is not functional.
Types of Shoulder Replacement
Computer Navigation
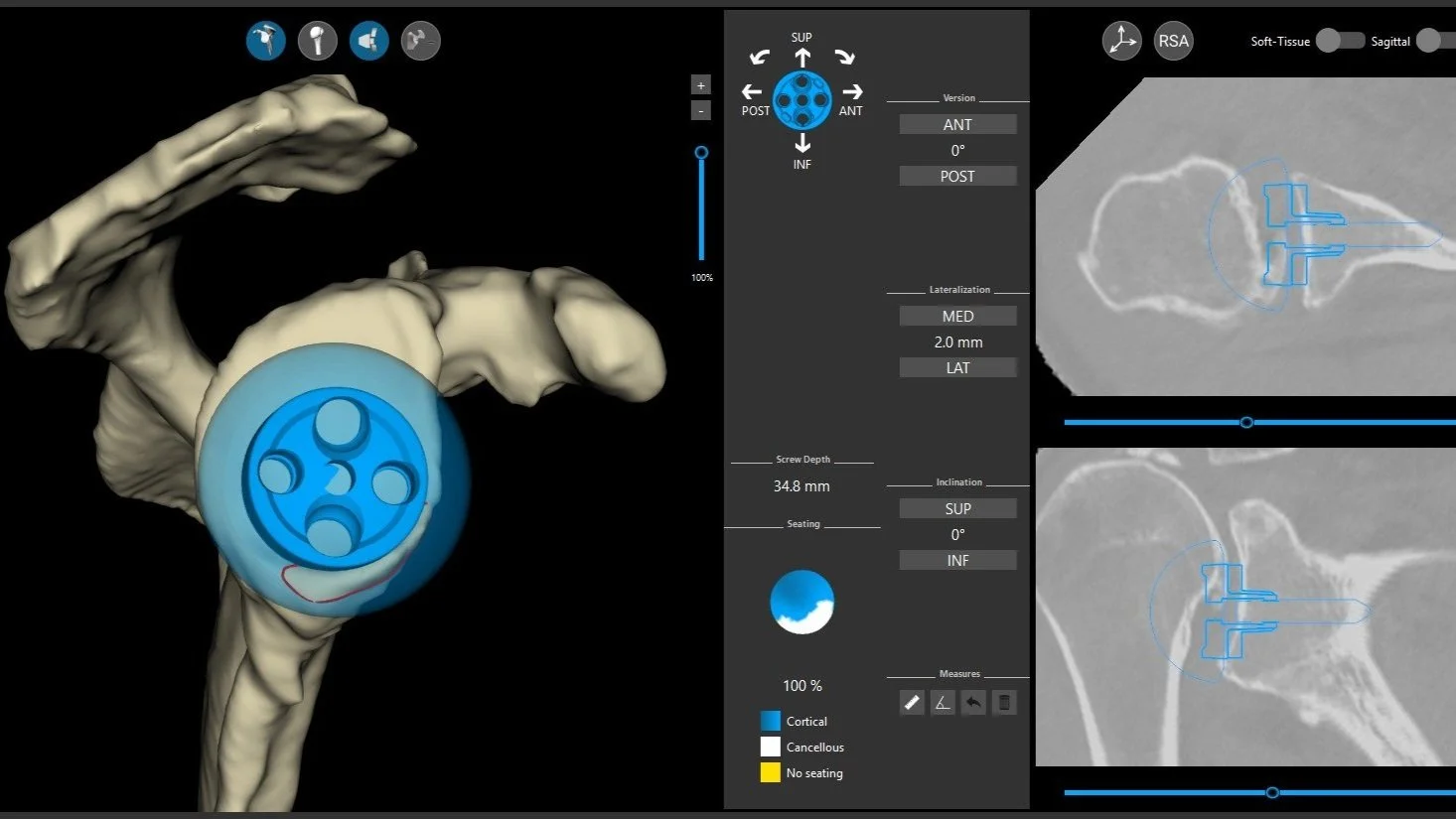
Dr. Ratner uses computer navigation on most of his shoulder replacements. Computer planning and navigation in total shoulder arthroplasty offer numerous benefits that enhance surgical precision, optimize implant placement, and lead to improved patient outcomes
Summary:
Computer navigation for shoulder arthroplasty leverages advanced imaging and real-time guidance to significantly enhance surgical precision and accuracy in implant placement. By creating 3D virtual models of a patient's unique anatomy and providing intraoperative feedback, this technology helps surgeons optimize glenoid component positioning, correct complex deformities, and reduce the risk of common complications like implant loosening and instability. While potentially involving a slight increase in surgical time and cost, the benefits of improved implant longevity and functional outcomes for patients, particularly in challenging cases, make computer navigation a valuable tool in modern shoulder arthroplasty.
Benefits of Computer Navigation Shoulder Arthroplasty:
Enhanced Precision and Accuracy
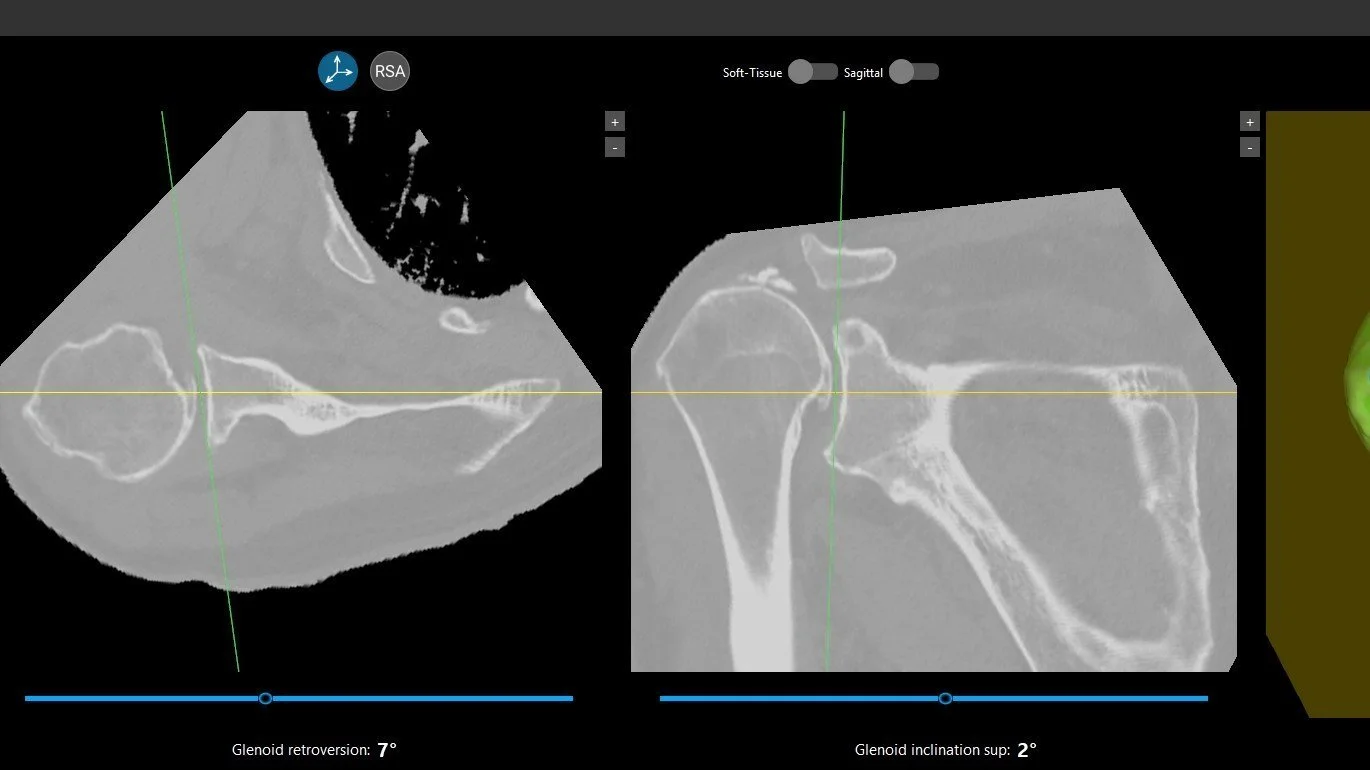
3D Visualization and Templating: Computer planning software utilizes detailed 3D computed tomography (CT) scans to create a virtual model of the patient's shoulder anatomy. This allows surgeons to precisely visualize complex bone deformities, assess glenoid wear patterns, and virtually "try on" different implant sizes and positions before the actual surgery. This level of detail is often impossible to achieve with traditional 2D imaging (X-rays).
Optimal Glenoid Component Placement: A significant benefit of computer planning is the ability to accurately plan the position, version (angle relative to the body), and inclination of the glenoid component (the socket part of the implant). Malpositioning of the glenoid component is a major cause of complications like instability, loosening, and scapular notching. Computer planning and intraoperative navigation systems help surgeons achieve more accurate and reproducible glenoid placement, even in challenging cases with severe bone loss or abnormal anatomy.
Improved Screw Placement: In reverse total shoulder arthroplasty, accurate placement of screws for the glenoid baseplate is crucial for fixation and longevity. Computer planning and navigation can improve the accuracy and precision of screw placement, leading to better stability.
Personalized Surgical Approach
Customized Implant Selection: By understanding the patient's unique anatomy in 3D, surgeons can select the most appropriate implant size, type (anatomic vs. reverse), and augmented components (wedges to correct bone defects) to best fit the individual's needs.
Addressing Complex Deformities: Computer planning is particularly beneficial for patients with significant glenoid deformity, severe bone loss, or previous failed surgeries. It allows for detailed planning to correct these issues, potentially reducing the need for bone grafting or optimizing its placement.
Optimizing Biomechanics: By precisely placing implants, computer planning aims to restore the natural biomechanics of the shoulder joint, which can lead to improved range of motion and function after surgery.
Improved Patient Outcomes
Reduced Complication Rates: More accurate implant placement can decrease the risk of post-operative complications such as dislocation, implant loosening, and scapular notching, which are often linked to technical errors in component positioning.
Longer Implant Lifespan: Precision in implant placement contributes to better long-term outcomes and may extend the lifespan of the implant by minimizing wear and stress on the components.
Enhanced Functional Outcomes: While long-term studies are still ongoing, improved implant positioning is expected to translate into better pain relief, increased range of motion, and overall improved patient satisfaction and quality of life.
Faster Recovery (potentially): By allowing for more precise and potentially less invasive techniques (though surgical time might initially be slightly longer with navigation until proficiency is gained), computer-assisted surgery may contribute to faster patient recovery.
Educational and Training Benefits
Improved Surgeon Understanding: The 3D planning software allows surgeons, especially those in training, to gain a deeper understanding of complex glenoid anatomy and pathology before entering the operating room.
Reduced Learning Curve for Complex Cases: While there is a learning curve for using the navigation systems, they can help surgeons, even those with less experience, achieve more consistent and accurate results in challenging cases